Is far-UVC right for you?
An adaptable business case template for using ultraviolet light to improve indoor air quality
Far-spectrum ultraviolet light is an emerging technology with the potential to dramatically reduce the indoor transmission of infectious diseases. While UV is obviously generally harmful, the 222nm wavelength available in new commercial devices cannot penetrate the outermost layer of skin, making it safe for use around humans while continuing to sterilise pathogens.
The technology and the growing body of science behind it have been well covered elsewhere (see here for a great introduction), but we’ve found a large information gap when attempting to build a business case for implementation. The idea might be attractive in principle, but how effective are these things on a cost basis? What sort of coverage should we aim for? How much value are we leaving on the table by not installing these things immediately? Can we trust supplier recommendations about what to install? (Spoilers: No).
Our findings are below, and a high-level far-UV cost/benefit model is freely available for download here1.
Key Findings
While far-UV shows considerable promise, we find that these devices, given current off-the-shelf pricing, provide limited direct value in most modern office environments. However, the value proposition is significantly higher in buildings with higher occupant densities, low airflow, and particularly in buildings with higher viral loads (e.g. schools in winter, hospitals, military barracks, and other locations where individuals are less likely to isolate when sick2), or where an extreme value can be placed upon people’s time (e.g. AI labs, executive government offices, civil defence coordination centres).
As the technology continues to mature, sales volumes increase, and economies of scale drive costs down, we expect these devices to become increasingly broadly viable.
Technology Overview
There are three broad categories of UV devices for improving indoor air quality:
In-duct installation. These longer-wavelength systems are harmful in the case of exposure, but can significantly reduce the infectiousness of recirculated air. Doesn’t affect direct transmission and is therefore generally less cost-effective3.
Upper-room ~254nm systems. Bathes the upper layer of the room in UV, reducing concerns of direct exposure at the cost of some efficacy—particularly in rooms with poor air circulation.
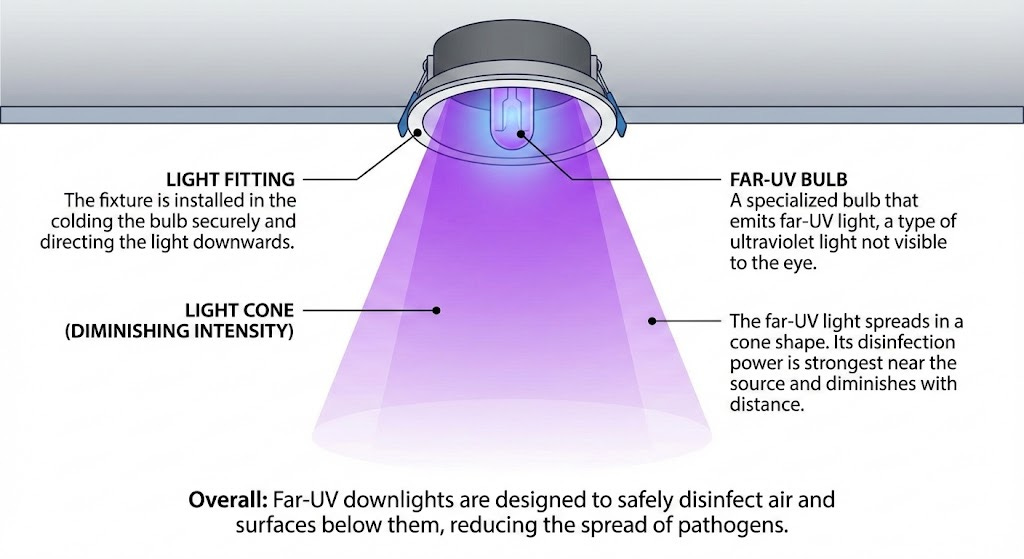
222nm downlight systems. This wavelength is too small to penetrate the outer skin layer, while remaining effective against viruses and bacteria. Strong evidence of safety for both skin and eyes, even during prolonged exposure. Most effective architecture, as it reduces direct transmission.
Model Overview
Suppliers tend to report the efficacy of their devices in terms of % reduction in infectious transmission, often quoting scientific studies that produced ~90% reductions under certain test conditions. Unfortunately, this is unhelpful for estimating real-world efficacy where room size, air flow, device coverage, etc., vary considerably.
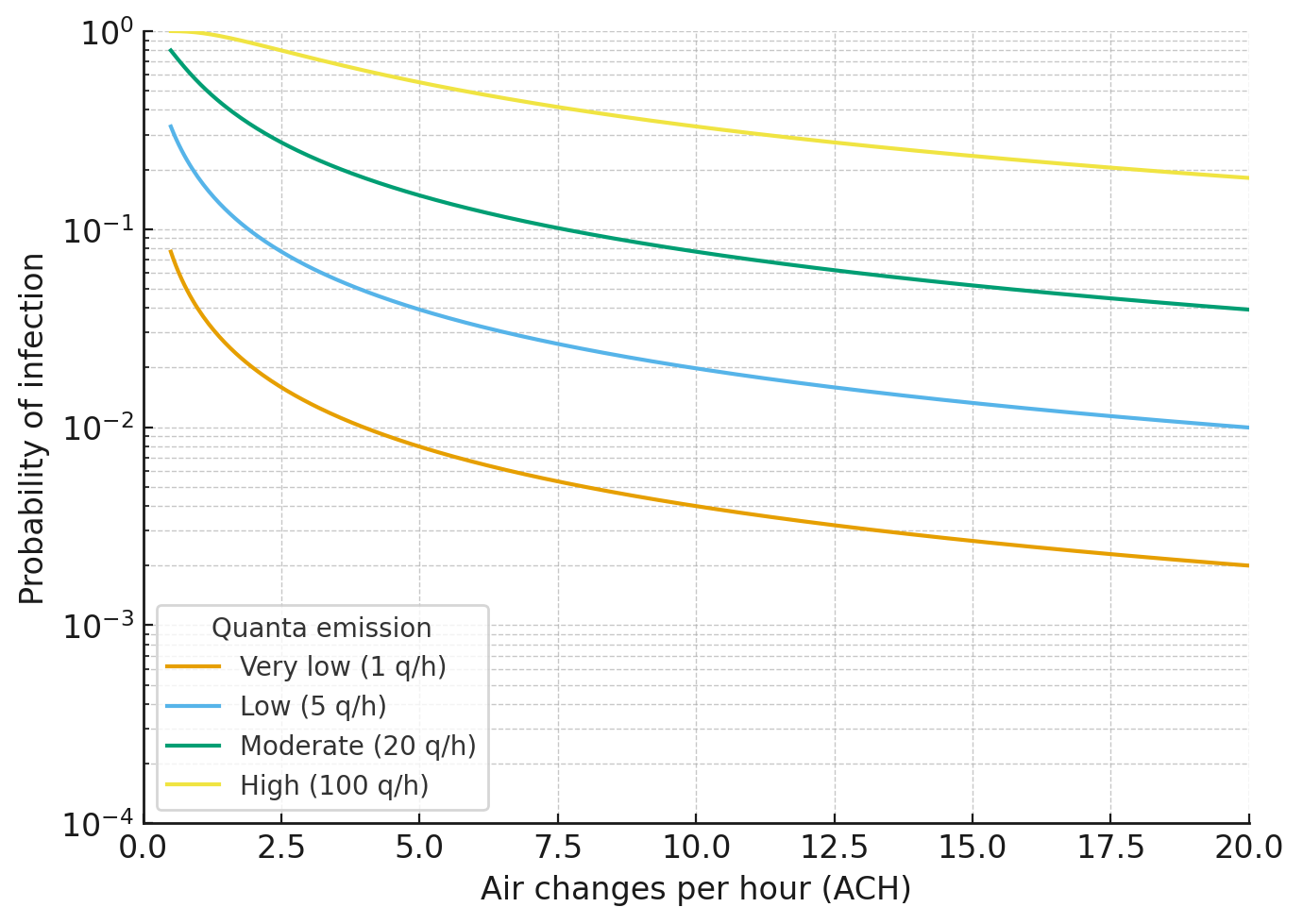
To make more site-specific predictions, we use the Wells-Riley model, widely used to estimate the probability of airborne infection of infectious diseases as a function of both the fresh airflow into a space (expressed in terms of air changes per hour, ACH), and how contagious the disease is for a given breathing rate (expressed in ‘quanta’ per hour). As you can see below, the model is one of diminishing returns to increasing airflow, particularly for the lower quanta typical of office environments4.
We can estimate the effects of UV by combining the relatively well-studied susceptibility of common respiratory pathogens to UV light together with the irradiance of different lamps at head height (a function of the wattage of the device, the breadth of the cone of light it emits, and the distance between the ceiling and the occupant). The result is a reduced probability of infection that can be expressed in terms of additional ‘effective air changes per hour’ (eACH).
By assuming that the predicted likelihood of infection from the model is proportionate to the average number of sick days resulting from respiratory infections contracted within the workplace/site, we’re able to compare different UVC arrangements against an observed base case (either using organisation-specific or broader economic data), and thus predict an annual reduction in sick days resulting from the installed system.
Finally, we derive a first-order estimate of benefits from the installed system by multiplying the predicted annual reduction in sick days by annual productivity (or for non-workers, any QALY-derived value can be used here5). By plotting this against estimated capital and operating costs, and adjusting for discount rate, we can plot how we expect each system to perform over time.
Assumptions
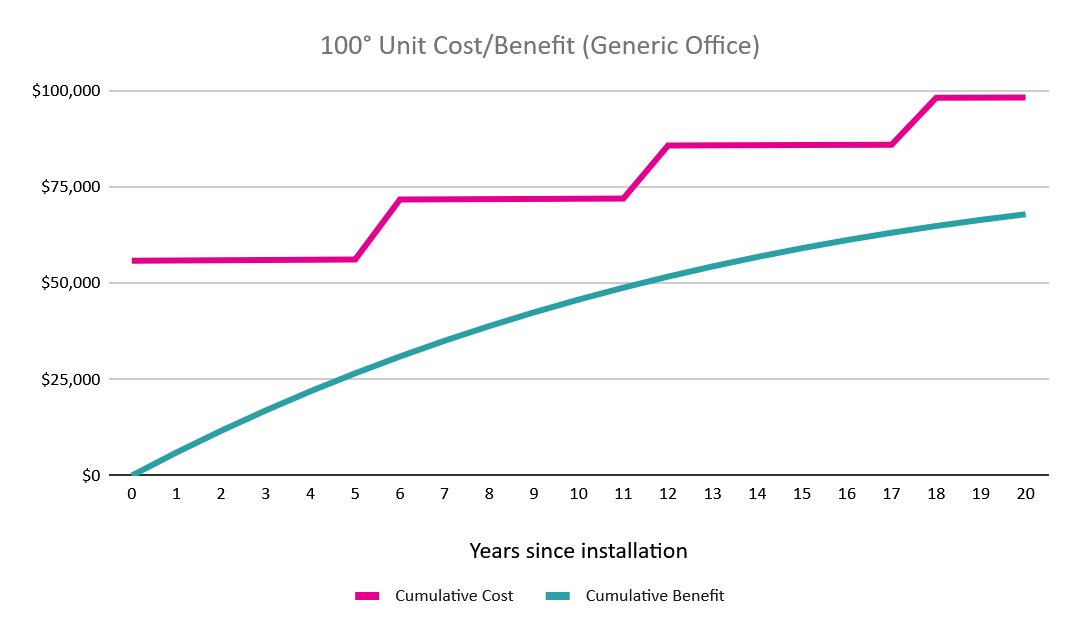
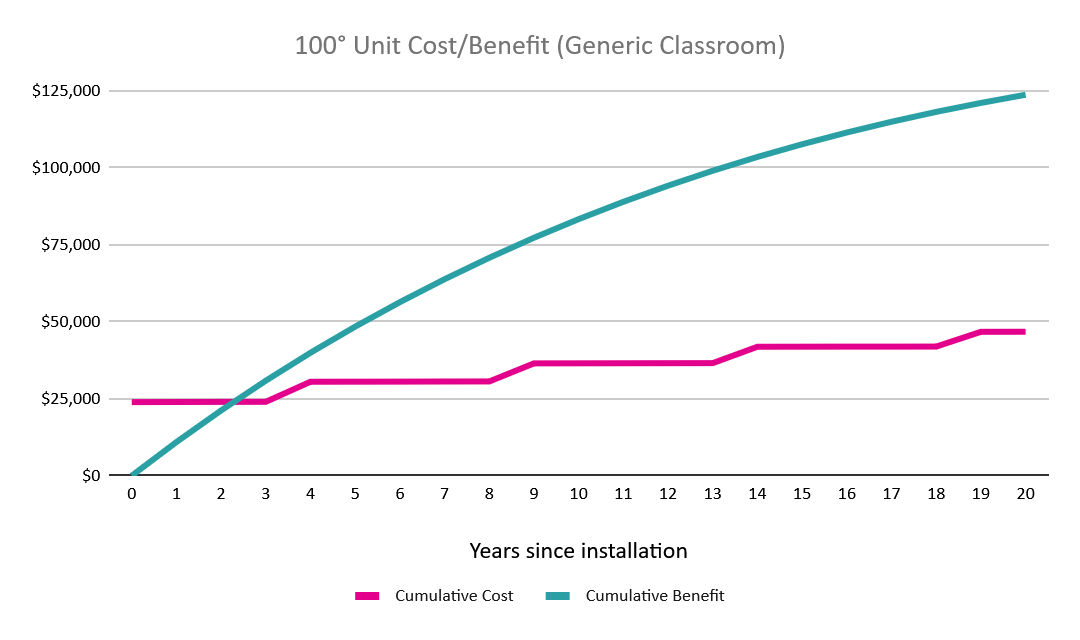
The suppliers we talked to operate on a model where users pay a relatively high upfront cost for the devices, but where the devices can be returned after bulb failure to be fitted with new bulbs at a lower cost. As the market matures, we expect other models to become more prevalent. In any case, the cost structure remains the same: high initial costs for both the fittings and the electrician’s installation, and lower stepped costs thereafter as the bulbs fail after approximately 10,000 hours of use. Lacking historical data about the useful life of the fittings, we’ve assumed a maximum of 20 years, by which time we expect the current generation of devices to either have been made obsolete or a new supply arrangement to be made.
UV-susceptibility varies considerably across pathogens. Some variants of the common cold are deactivated roughly 3x faster by a given UV irradiance than the H1N1 flu. A complete model would model each pathogen individually based on both its susceptibility and impact on health, then sum results across all of these pathogens according to their local prevalence and occupant vaccination rates. Unfortunately, limited reliable pathogen susceptibility data makes such an approach difficult. Instead, we’ve simply taken the mid-point of the observed range, since even relatively sparse far-UV installations provide very high eACH (typically 50+ in covered areas, depending on the height of the room). Since there are diminishing returns from increasing ACH under Wells-Riley, sensitivity analysis shows using even the extremes of the susceptibility range (e.g. H1N1) results in only a 3% variance in predicted infection reduction in most typical use cases/building environments.
Building layouts obviously vary considerably; no generic model can cover every case. While users can manually input coverage statistics into the spreadsheet, the default assumption, given the typically low marginal benefit of increased irradiance, is a system of tightly packed non-overlapping coverage at head height. This results in ‘dead-zones’ of limited coverage, such as at the sides and corners of the room. We assume that care will be taken during detailed design to ensure that these zones are located in low-traffic areas, such as above storage cupboards and other areas where it is either impossible or unlikely for people to congregate and transmit disease.
Results
With little information available about system design at the outset of our study, we had little to go on beyond scientific studies and supplier recommendations, both of which are essentially cost-insensitive and prone to recommend far higher device coverage than is optimal from a cost-benefit perspective.
With diminishing returns to intensity, we find that wider 100° aperture devices outperform tighter 60° devices in all but the most extreme of circumstances (e.g. in the exemplar office setup, annual productivity of above $1.8m NZD per person is required before returns increasingly accrue to the 60° device).
Similarly, reference designs often create overlapping coverage at desks, gathering areas, and other high-traffic areas in order to maximise protection. We find the coverage of a single downlight to be more than sufficient, providing protection equivalent to a quadrupling of typical modern office airflows. That said, depending on the layout of the building, some projects may wish to introduce additional lamps to avoid ‘dead zones’ in key areas.
Far-UV tends to be lower value for offices, as they tend to be better ventilated, more sparsely occupied, and surprisingly uncontagious (at least in places with generous sick-leave allowances)6. However, we see significant potential for far-UV in environments like classrooms, which tend to be much more crowded and (sadly) poorly ventilated. Here, and in any environment where occupants are unlikely or unable to self-isolate (preschools, hospitals, military barracks, etc.), we see considerable returns on investment.
End Notes
Since the power draw of these devices is no larger than a standard incandescent light bulb, operating costs are very low relative to capital. Safely and reliably producing far-UV is considerably more involved than visible spectrum light, but from a fundamental materials standpoint (ignoring IP and so forth) is likely no more than a single order of magnitude more costly than visible spectrum, rather than the 2+ orders of magnitude price differential we see currently. Thus, if the market for far-UV matures to the point where these devices are simple high-volume commodities, then these devices could become almost universally beneficial.
Finally, it’s worth noting the rather mercenary nature of our model, focusing only on first-order benefits to the installing organisation. However, each infection prevented as a result of far-UV is, on average7, another infection prevented within the population. Widespread installation of these devices could dramatically reduce disease prevalence in a non-linear fashion, creating widely distributed benefits for our entire society.
Thanks to Gavriel Kleinwaks from 1Day Sooner, who introduced the tech to me at Manifest in June, and was generous with her time answering my questions.
To use the model, click ‘file’ at the top left, then download yourself a copy. The model has been into the public domain via a Creative Commons zero licence.
Schools are particularly bad here. Not only are children obviously much more likely to be sick over winter, but older classrooms, usually lacking HVAC systems, tend to have particularly poor airflow during winter, when windows are shut to retain heat. In summer, where windows are thrown open to aid cooling, the air can be replaced 5 times each hour. In winter, this can drop to 0.5, dramatically increasing infection rates.
Since in-duct systems are typically retrofitted into an existing HVAC system, the costs involved are extremely variable, dependent on ease of access, contractor familiarity, etc. Unlike other options where costs are highly predictable, those interested in exploring in-duct would need to obtain quotes in order to get even a rough order understanding of potential cost/benefits.
Quanta estimates range considerably. This study estimates up to 270 for highly infectious diseases like Covid when singing or speaking loudly, 42 for quiet speaking, and 3 for breathing at rest. You might recall that very few people contracted Covid on aeroplanes—passengers tend to speak quietly if at all, and the design of aeroplanes forces fresh air through the cabin every few minutes (cruising ACH is typically around 25), resulting in very low infection probabilities. On the other hand, many would subsequently become infected in the airports and hotel lobbies, where speaking is more common, and airflow is much more limited.
Another assumption here is that the impact of infection can be measured purely in terms of sick days. Thanks to the many miracles of modern medicine and antibiotics, this is mostly true for adults and all but the youngest children. Sadly, it’s not true for everybody, and an adjustment should be made here to account for mortality risk in areas like rest homes, hospitals, and other locations with immunocompromised occupants.
See details of our estimate of office contagiousness on the ‘Calcs’ page of the model.
If a disease is in roughly steady-state with the human population (e.g. a population contracts roughly the same number of common cold infections each year), then each infected person infects one other on average. However, Covid-19 data and common sense both suggest a heavily right-skewed distribution where most infections are transmitted to nobody, while a few infections result in ‘super-spreaders’ events infecting a great many others. Most salaried professionals with ample sick leave stay home when they’re sick. Many diseases, by contrast, spread rapidly through childcare centres. There’s consequently asymmetric second-order upside to introducing far-UV to these sorts of locations.


Nice work on this! Mostly congruent with my views, although I think due to the requirement of high-quality quartz glass and time on expensive sputtering machines for the filters, it's unlikely that current-gen far-UVC fixtures based on krypton-chloride lamps will sell for much less than ~$60-$100. So a x5 cost drop, but not orders of magnitude. Future solid state devices based on second harmonic generation can maybe do better, if there's a business case for the capital investmen.
I'm surprised that you find the 100° aperture lamps do better than the 60° and suspect there is a mistake in the analysis. The 100° b1.5s have better coverage and are less reliant on air movement, but have 1/4 of the output and documented lifetime issues. There's no way that's offset by better coverage alone.
I also wonder what your assumptions are for upfront costs. I generally recommend 1 corner-mounted b1 lamp for a 250 sq ft space (100mW->~0.5 uW/cm2 average fluence), which can be had for $500 plus shipping and doesn't necessarily require installation by an electrician. Does that still come out in the red for offices in your analysis?
Spot on; your cost-benefit dive really highlights far-UVC's clear value for schools and AI labs where the stakes are higher.